Escherichia coli
- Genel Mikrobiyoloji

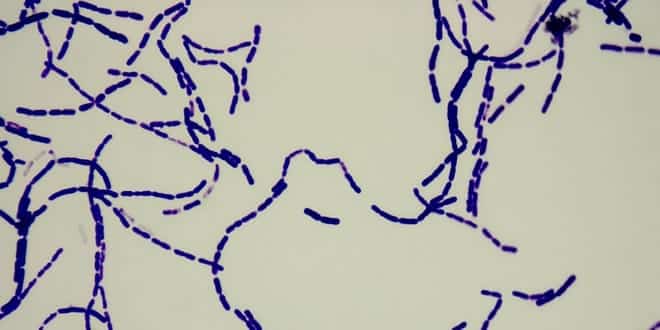
Gram Stains of Bacteria
Gram Stains of Bacteria Escherichia coli, Klebsiella pneumoniae, Enterobacter aerogenes, Staphylococcus aureus, Staphylococcus epidermis, Bacillus subtilis, Bacillus cereus, Bacillus megaterium, Bacillus megaterium,…
- Genel Mikrobiyoloji

Enterohemorrhagic Escherichia Coli Infections
In today’s presentation we will cover information regarding Escherichia coli (E. coli) and its epidemiology. We will also talk about the history…
- Hijyen ve Sanitasyon

Gıda Kaynaklı Hastalıklar ( Fırat ÖZEL )
GIDA KAYNAKLI HASTALIKLAR Fırat ÖZEL, Gıda Mühendisi 2006 Amaç Eğitimin amacı : Gıda sanayinde hataların sonuçlarını belirtmek. Yaptığımız işin ciddiyetini göstermek. Dikkatli…
- Genel Mikrobiyoloji

Differential Staining Gram Staining, Endospore Staining & Capsule Staining
Purpose: To learn what is differential staining and its purposes To perform three types of differential staining: Gram staining, Endospore staining and…
- Genel Mikrobiyoloji

Escherichia Coli ( İlkay ÜNAL )
Genelde E. coli kısaltması ile veya koli basili olarak bilinen Escherichia coli (okunuşu Eşerişiya koli), memeli hayvanların kalın bağırsağında yaşayan faydalı bakteri…